Advancing Immunotherapy Testing with Functional Antigen-Specific T Cells
Watch our latest Labroots webinar exploring next-generation solutions that enhance immunotherapy evaluation and accelerate translational research.

|
January 16, 2026
|
7 min read
Watch our latest Labroots webinar on Antigen-Specific T Cells, presented by our Scientific Director of Innovation, Dr Emilio Cosimo, and BioIVT's Senior Scientific Advisor for Cell and Gene Therapy, Kevin King.
Key points include:
- The role of antigen-specific T cells in adaptive immunity and their application in immunotherapy testing
- Comparison of TCR-T and endogenous T cell generation strategies, including challenges and rescue approaches for exhaustion
- How RoukenBio and BioIVT capabilities enable scalable, flexible platforms for translational research and collaboration for researchers across autoimmunity, immuno-oncology and complex cell therapy development
What are the key challenges in immunotherapy and autoimmunity?
Immunotherapy has transformed cancer treatment, but significant challenges remain.
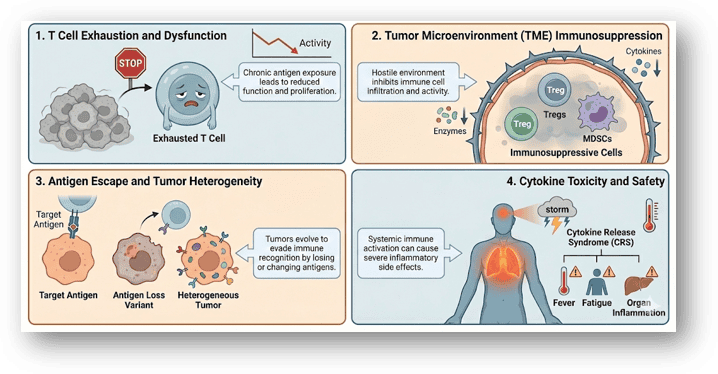
One major challenge is T-cell exhaustion, which is driven by chronic antigen exposure and limits the effectiveness of therapies such as CAR-T and checkpoint inhibitors. Tumour microenvironment is another key barrier for therapeutics, as it's a complex immunosuppressive ecosystem that includes regulatory T-cells and suppressive cytokines, making it difficult for T-cells to function and infiltrate. Tumour heterogeneity, mutations and antigen loss can lead to relapse even after initial success. And finally, cytokines’ cytotoxicity presents safety concerns and can limit applicability of these therapies. So all current immunotherapies need to consider all of these challenges and in this context antigen-specific T cells are essential for testing new drugs.
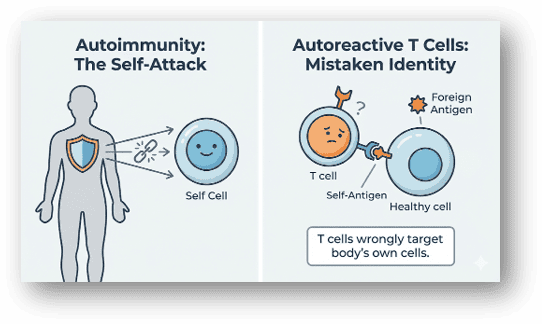
Autoimmunity presents a different set of challenges. Autoreactive T cells become activated when immune tolerance is disrupted, resulting in the failure of mechanisms that normally stop the immune system from attacking the body. Therapeutic strategies may target T-cells directly in T-cell-driven diseases like in MS or Type 1 diabetes, or B-cells in conditions involving autoantibodies like in SLE and rheumatoid arthritis. Innovative approaches such as CAR-T therapy are being explored to eliminate pathogenic cells for autoimmune diseases such as lupus and rheumatoid arthritis. Antigen-specific T cells are crucial tools for developing innovative therapies that restore tolerance without compromising immune defence.
Antigen-Specific T Cells (ASTCs) in Adaptive Immunity
Antigen-specific T-cells are a cornerstone of the adaptive immune system. Each T-cell expresses a unique T-cell receptor (TCR), enabling it to recognise specific antigens presented by the MHC or HLA complex. These cells are vital for fighting infections, eliminating cancer cells, and maintaining immune memory.
Understanding antigen-specific T-cells biology is key to developing targeted therapies for cancer, infection disease, and autoimmune disease. Advances in T-cell engineering are opening new avenues for treatment, however, the low frequency of these cells in peripheral blood remains a challenge, from both research and clinical applications.
Key T-cell Subsets in Immunotherapy Testing and Autoimmunity:
- Helper T cells (CD4+): coordinating immune responses via cytokine secretion, activating B cells and macrophages. They recognise peptides presented by HLA class II molecules.
- Cytotoxic T cells (CD8+): directly killing infected or malignant cells. They recognise peptides presented by HLA class I molecules.
- Regulatory T cells (Tregs): maintaining immune homeostasis and self-tolerance by suppressing excessive immune response like effector T cell activity.
- Memory T cells (usually CD4+): persist after infection to facilitate rapid secondary response upon antigen re-exposure.
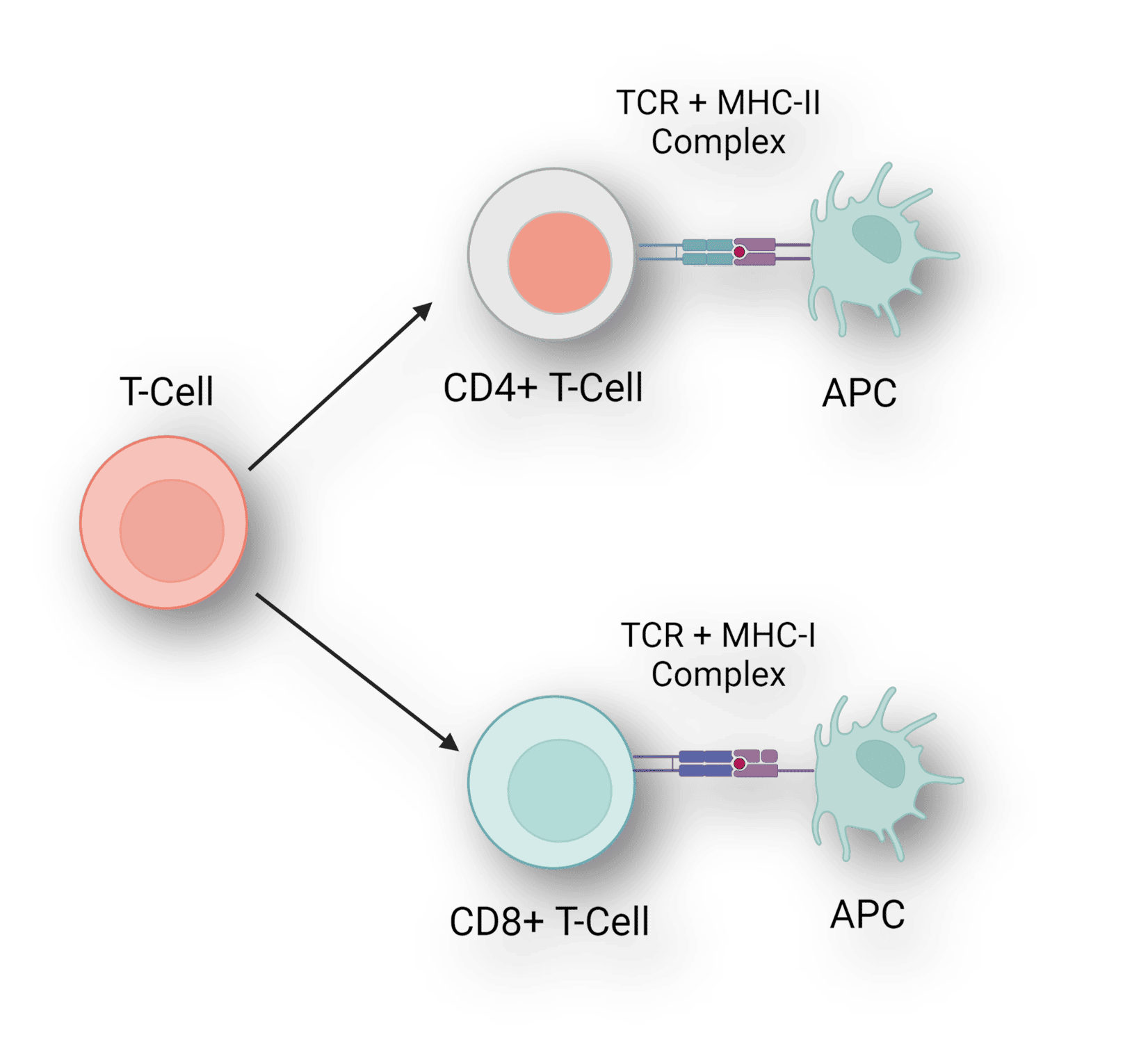
Image created via using BioRender.
The diversity of T-cell receptors is vast; up to 1015 possible combinations, with only about 106 to 107 being present in any individual. Adults have around 4 × 1010 CD8+ T cells, but each antigen-specific clone is relatively rare. This low frequency makes it challenging to utilise these cells in research and therapy, and tracking these rare cells is crucial for understanding disease and improving diagnostics and treatments. Therefore, having scalable sources of antigen-specific T-cells is crucial for drug testing, drug discovery, and to model T cell exhaustion.
TCR-T Cells for Targeted Immunotherapy Testing and Autoimmunity Research
TCR-T cells are T-cell engineered to express specific TCR for targeted therapy and research. This approach allows us to create cells with defined specificity, overcoming the reliability of naturally occurring antigen-specific T-cells. TCR T-cells are a powerful tool for both therapy and drug discovery, allowing us to test immunomodulators and model disease.
T-cell therapies involve engineering patient T-cell lymphocytes, usually to express antigen-specific TCR, enabling the recognition of intracellular tumour-derived peptides presented by the MHC molecules. Unlike CAR T-cells, which target surface antigens, TCR T-cells can access a broader range of tumour-associated antigens, including cancer testis, antigens, and neoantigens. However, there are challenges for these therapeutics. There is an issue of specificity, which is essential to avoid off-target toxicity. Persistence is needed for durable responses, and continuous antigen exposure can lead to T-cell exhaustion
Take your Immunotherapy Testing to the Next Level with Functional Antigen-Specific T Cells
TCR-T cells are not only a valuable therapeutic modality, but also a valuable tool for testing immunomodulating therapies designed to either boost or suppress immune activity. As previously mentioned, a major challenge is having sufficient numbers of standardised antigen-specific T cells ready for immunotherapy testing. To address this, we created transgenic 'Thaw-and-Go' TCR-T cell banks that provide a scalable, ready-to-use solution for innovative drug and therapeutic developers in autoimmunity, immunooncology and beyond.
Join our community of curious minds on LinkedIn
🗓️ Stay informed with our monthly scientific newsletter, published on LinkedIn on the last Wednesday of each month.
These editions bring you the latest in drug development breakthroughs, industry trends, and expert insights from the brilliant minds at RoukenBio.
Subscribe today on LinkedInPropel your drug discovery with Functional Antigen-Specific T cells
See how our Antigen-specific T-cells work in our ASTC exhaustion model case study offering you key insights.
Access the case study