Inside Innovation: A Conversation on the Future of Cell Therapy
The world of advanced therapies is evolving rapidly, with CAR-T and allogeneic cell therapies leading the charge in transforming how we treat complex diseases. In this exclusive interview, Dr. Emilio Cosimo, Scientific Director of Innovation, shares expert insights into the breakthroughs, challenges, and future potential of these cutting-edge treatments - and how innovation is paving the way for broader access and impact.

|
August 25, 2025
|
12 min read
In recent years, the field of advanced therapies has undergone a remarkable transformation, driven by breakthroughs in genetic engineering, immunology, and regenerative medicine. At the forefront of this revolution are Advanced Therapy Medicinal Products (ATMPs), a class of cutting-edge treatments that harness the power of cells, genes, and tissues to tackle diseases once thought untreatable.
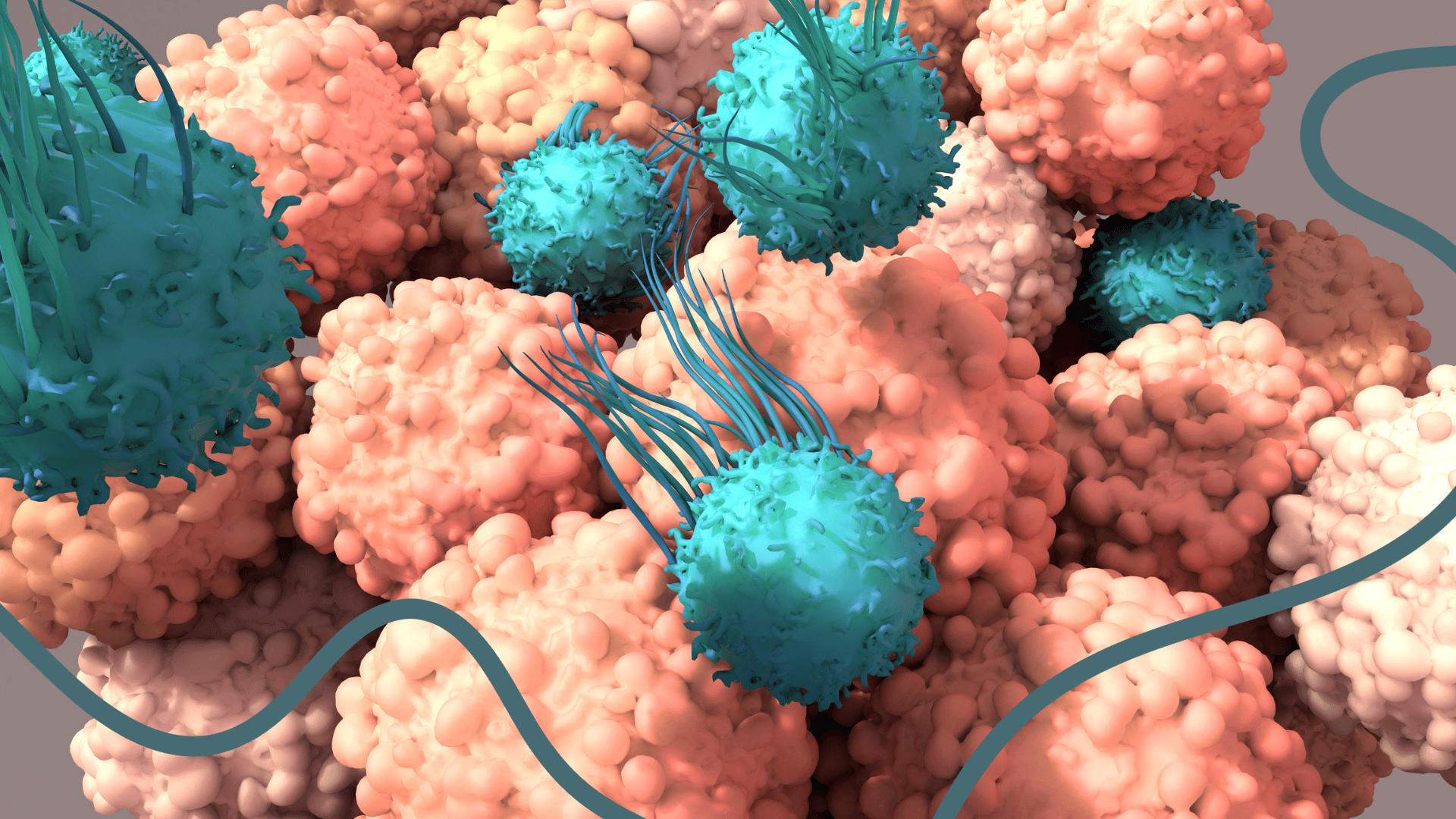
Among the most promising ATMPs are CAR-engineered immune cells, particularly CAR-T cell therapies, which have shown unprecedented success in treating certain blood cancers. Meanwhile allogeneic cell therapies, which use donor-derived cells, are emerging as scalable, off-the-shelf solutions that could dramatically expand access to these life-saving treatments.
To explore the evolving landscape of cell therapies, we spoke with Dr. Emilio Cosimo, our Scientific Director of Innovation here at RoukenBio. In this insightful conversation, we delve into the challenges, opportunities, and future directions of CAR therapies, the promise of allogeneic platforms, and the role of innovation in shaping the next generation of cell-based treatments.
ATMPs – The Benefits, Challenges and Future Discoveries
ATMPs, especially CAR-Ts, have the potential to be curative and can be designed to be personalised. Cell therapies present unique complexities mainly because they are based on living cells unlike biologics or small molecules. They therefore can be defined as personalised medicine.
Bringing CAR-T to the clinic is challenging, with proving clinical efficacy in solid tumours as the main hurdle. Investment in biotech is currently limited, and companies must demonstrate clinical signals (at least in early phase 1 or small trials) to attract further funding. Despite promising preclinical data, there is a lack of financial support for phase 1 trials, and investors demand clinical results before committing funds. Nonetheless, there are potential strategies to break this cycle. Emilio went on to say:
“I think collaborations, especially with institutions and university or research hospitals, have the potential to address this gap. These organisations offer their own products and therapeutic innovations, which could facilitate bridging existing divides. A shift in the financial environment would also be beneficial, as successful outcomes could stimulate additional interest and engagement in the field.”
We asked Emilio what he thinks the future trends in ATMPs are and how they will impact clinical development. He continued, his interest in the subject evident:
"What has become apparent, particularly in the field of CAR-T, is a significant shift toward extremely rapid and abbreviated manufacturing timelines. Currently, ‘from vein to vein’, the process could require five to six weeks due to the necessary steps of procuring starting materials, manufacturing, testing, and product release.
Emerging trends suggest that manufacturing process duration may now be shortened to only a few days, thereby reducing the overall timeline from five or six weeks to approximately two to three weeks.
Additionally, advances in process development automation are contributing to these reductions, both by minimising points of failure and by increasing product consistency. The move towards more automated, less manual processes is expected to enhance efficiency, decrease risk, and ultimately have a positive impact on production timelines and cost of goods."
As we look to the future of ATMPs, CAR T-cell therapies offer a compelling glimpse into what's possible when cell engineering meets precision medicine.
Exploring Target Selection, In Vivo Strategies, and the Future of CAR-T Therapy
When assessing an optimal CAR target, one of the most essential features is a high signal-to-noise ratio, specifically, a clear differential in expression between tumour and normal tissue. If a validated target demonstrates a pronounced distinction in expression levels between malignant and surrounding healthy tissue, the process of product design and development is significantly streamlined. Conversely, when the difference in expression between tumour and normal tissue is minimal, more complex strategies may be required.
Another important aspect is the stability of antigen expression. In cases where the antigen remains consistently detectable without escape, the tumour is not selected for reduced or negative antigen levels, as seen with CD19 and CD20 in haematological cancers. Additionally, antigens present in the tumour microenvironment, including those expressed by non-cancerous associated cells, can be relevant and exploitable. Together, these features help ensure both the specificity and durability of CAR-based treatments.
In solid tumours, identifying suitable CAR targets is hindered by the complexity and effort required for comprehensive target validation. Potential targets can be identified through genomic and proteomic screening; however, confirming their suitability requires extensive data analysis and validation using histology and human biopsies. This process involves evaluating expression within the tumour, antigen accessibility, stability, and appropriateness for CAR targeting.
Each candidate undergoes proof-of-concept studies to determine therapeutic potential, which involves significant time and resources. AI-driven methods may assist in data interpretation and facilitate target discovery, yet experimental validation remains necessary. The combined scientific and practical demands make target validation a major challenge in the development of CAR therapies for solid tumours.
"In my opinion, finding a potential target involves more than comparing tumour vs normal tissue; it's also about identifying antigens that can be targeted by a CAR constraint."
When it comes to innovation in CAR-T, we wanted to know: what’s catching our new Scientific Director’s attention? Here’s what Emilio had to say:
“In vivo CAR-T presents a potentially transformative approach. First noted in 2022, its primary advantage lies in reducing the need for extensive ex vivo manufacturing, which may result in a process that is more efficient, cost-effective, and timely. Although definitive evidence regarding its efficacy is still pending, clinical trials have already commenced. It remains essential to evaluate its potential benefits, but both theoretical and preclinical data are currently promising.
Unlike conventional methods where cells are harvested from patients or suitable donors and then processed (a process that incurs significant time and expense) in vivo CAR-T involves encapsulating a transgene within a gene delivery vector, akin to gene therapy. In this paradigm, the human body functions as a manufacturing incubator, thereby mitigating many of the risks and costs associated with traditional ex vivo CAR-T therapies. While further validation is necessary, the scientific rationale behind this approach appears compelling.”
Personalised, patient-specific CAR therapies are a fascinating area of innovation, but scalability remains a challenge. Autologous cell therapies have already demonstrated the potential of personalised approaches. However, in the allogeneic space, where therapies are designed for broader use across multiple patients, true personalisation is still in its early stages.
Most CAR designs today aren't customised for individual patients, which limits how ‘personalised’ they can be. That said, in vivo CAR-T therapies may offer a more scalable route to personalisation, as gene delivery systems and transgenes could be more easily adapted to suit specific patient needs. While the concept is proven, especially in autologous therapies, widespread scalability of personalised CAR treatments is likely still a few steps ahead.
Defining Potency in CAR-T and Engineered Cell Therapies
Potency in cell therapies like CAR-T is a nuanced concept that depends heavily on the product’s mechanism of action. For CAR-T therapies, potency has traditionally been defined by the ability to kill target cells. However, this definition is evolving. Other factors such as cytokine expression, proliferation, persistence in the body, and time to exhaustion are increasingly considered part of a broader matrix approach to potency.
With clear enthusiasm, Emilio continued:
“To define potency effectively, it’s essential to deeply understand the therapeutic product. This means identifying all potential mechanisms of action and determining which are most relevant to clinical outcomes. A wide-net strategy - examining multiple parameters and narrowing down to the most consistent and impactful ones - can help pinpoint the most meaningful potency indicators.”
Key Characteristics of a Robust Potency Assay for Cell Therapies
A robust potency assay must be directly relevant to the therapy’s mechanism of action. Regulatory agencies emphasise the importance of having a direct readout of this mechanism. In cases where direct measurement is challenging, especially in complex cell therapies, validated surrogate markers can be used to build a reliable potency assay. Demonstrating his passion for the field, he went on to say:
“The foundation of a successful potency assay lies in a thorough understanding of how the therapeutic works. This enables the identification of biomarkers that correlate with the mechanism of action, simplifying assay development and improving the likelihood of successful validation.”
Ultimately, a potency assay must be fit for purpose and meet standard validation criteria, including linearity, robustness, reproducibility, and sensitivity within the limits of detection. These principles apply broadly across pharmaceutical research, not just within cell therapy.
Reimagining Potency Testing in CAR-T: From 2D Assay Systems to 3D Organoid Models
Given how critical antigen specificity, stability, and accessibility are in identifying ideal CAR targets, especially in solid tumours, it's clear that more predictive preclinical models are essential. This is where organoids and 3D tumour models come into play, offering a more physiologically relevant environment to assess CAR potency, antigen expression dynamics, and potential off-target effects. Picking up momentum, our new Scientific Director of Innovation added:
"I strongly support the use of organoid and 3D tumour models for developing potency assays in solid tumour CAR therapies, as this approach represents a promising direction for the future. However, it will likely be some time before we see validated potency assays implemented, since integrating such an assay into the release testing for a product requires a highly robust development and qualification process.
Fundamentally, it is crucial to confirm that the assay is fit for its intended purpose. Following this, validation involves a stringent series of procedures to ensure not only suitability but also the capability of the assay to accurately indicate both the functionality and potency of the product."
Currently, many in the field are already grappling with the limitations of traditional 2D systems when it comes to assessing the potency of cell therapies, which are inherently more complex than biologics or small-molecule drugs. Cell therapies can exert their effects through multiple mechanisms of action, making it difficult to define potency in a way that reliably predicts clinical efficacy.
At present, potency assays are primarily designed to establish product attributes for release, rather than to serve as relevant indicators of therapeutic performance. As a result, there is often little correlation between the assay characteristics and the clinical outcomes observed. While some companies with large patient datasets are beginning to retrospectively analyse the predictive value of their potency assays, the field still has considerable progress to make. Nevertheless, organoids and other 3D tumour models represent a promising direction for developing more physiologically relevant and predictive potency assays.
Challenges and Opportunities in Scaling Allogeneic Cell Therapies
One of the major challenges in scaling up allogeneic cell therapies for mass production is donor selection. Identifying suitable donors requires significant time and resources, not just from a manufacturing perspective, but also to meet varying regulatory standards across different regions. What qualifies as a ‘safe donor’ can differ widely depending on geographical territory, making donor accessibility, selection, and regulatory compliance key hurdles to overcome.
“Despite challenges, the opportunities are substantial”, continues Emilio. “Allogeneic therapies offer the potential to dramatically reduce costs by enabling upfront manufacturing and batch release. With an off-the-shelf product, the entire process, from production to release testing, can be completed in advance. This allows for rapid deployment to clinical sites, reducing the time from order to delivery from weeks to just days".
Cost Effectiveness and Faster Deployment of Allogeneic Therapies
Compared to autologous therapies, allogeneic cell therapies offer considerable cost advantages. These savings, potentially 10 to 20 times lower, depend on the complexity of the manufacturing process and the level of R&D investment.
“One of the biggest cost-saving factors is logistics. Instead of a ‘vein-to-vein’ process, allogeneic therapies follow a ‘box-to-vein’ model, where treatments are produced and stored in advance, ready for immediate use.” - added Emilio.
This shift not only reduces costs but also accelerates deployment. With pre-manufactured products, clinical trials and treatments can proceed without the delays associated with patient-specific manufacturing. This streamlined approach enhances scalability and makes allogeneic therapies a promising solution for broader patient access.
From Oncology to Autoimmunity: Resetting the CAR-T Landscape Through Innovation and Partnership
As the field of cell therapy continues to evolve at pace, the future relies not only on scientific innovation but also on how we navigate the complex regulatory landscape, especially with emerging platforms like allogeneic and in vivo CAR-T therapies. The traditional autologous allogeneic ex vivo CAR-T is going through a reset. Many companies are now shifting their focus from oncology to autoimmune diseases, driven by growing interest and investment in the latter.
This pivot is particularly evident in CD19-targeted therapies, which have shown promise beyond haematological cancers. Ex vivo approaches, both autologous and allogeneic, are increasingly being explored in autoimmune indications to generate clinical data that can attract further investment. This renewed momentum may eventually feed back into oncology research. Meanwhile, in vivo CAR-T technologies, though still relatively new, are also beginning to follow this trend. Most of these programmes remain concentrated in haematological cancers or autoimmune diseases, with CD19 continuing to be a central target across both areas.
"I anticipate that the near future will involve extensive research and data generation. There is hope for groundbreaking therapies targeting autoimmune diseases. Once these developments are well-established and adequately funded, it is expected that attention will shift back to addressing other challenging conditions, such as solid tumours." – Emilio reflected.
These therapies can be advanced; however, it is important to highlight the necessity for innovation and collaboration to achieve this. With the current lack of funding and nervousness from investors, collaborations and consortiums are of the upmost importance. No one will be able to do these complex therapies on their own. Whether in industry or academia, organisations are actively seeking new technologies to license and integrate into their pipelines.
“One of my primary responsibilities is to bridge the gap between customer requirements and our services. By identifying their needs, we can effectively deliver and expedite solutions that support their objectives.”
With expertise in combined therapeutic approaches, we are well-positioned to contribute to this collaborative effort and remain committed to identifying and delivering what the field requires.
Join our community of curious minds on LinkedIn
🗓️ Stay informed with our monthly scientific newsletter, published on LinkedIn on the last Wednesday of each month.
These editions bring you the latest in drug development breakthroughs, industry trends, and expert insights from the brilliant minds at RoukenBio.
Subscribe today on LinkedInReady to innovate the future of CAR T cell therapy?
See how our specialised expertise can fast-track your progress. Dive into two compelling CAR T case studies and find out how our advanced platforms and comprehensive capabilities empower your cutting-edge cell therapy projects.
Access the CAR T slides

